Do you listen to your doctor?

Forgetting to take medicine, only taking half a tablet or postponing a doctor’s appointment doesn’t cause any problems, right? In fact, it does. Successful treatment requires more than just the right medications. We talked to Lothar Roessig, cardiologist and Head of Clinical Development in the Therapeutic Area Cardio-Renal at Bayer, about why it is so important to consult your doctor regularly and follow their prescriptions and what impact the coronavirus pandemic is having on cardiovascular diseases.
Mr. Roessig, what does treatment adherence mean?
Check-ups, timely diagnosis, regular reviews and conversations with your doctor and especially taking drugs properly – all of this counts as treatment adherence and has a decisive influence on the success of treatment.
Drugs are carefully tested in studies for years before they are launched on the market for use in patients. In the approval studies, great care is naturally taken to ensure that the patient takes them regularly and in the correct dosage – and only under these circumstances can they bring about the desired success. For that reason, the intake of the drugs in their application should of course ideally be implemented in exactly the same way.
When prescribing medication, doctors usually base their decisions on the guidelines and recommendations of professional societies and regulatory authorities, which, in turn, are based on clinical studies and are constantly being adapted to reflect new findings. It is therefore important to speak to your treating doctor regularly and to follow their instructions.
Why is treatment adherence so important, especially for patients with cardiovascular diseases?
For cardiac patients, regular check-ups form part of the treatment repertoire. This is especially important in order to detect changes in the course of the disease over time and thereby avoid emergency situations such as hospitalization. With heart failure and blood-thinning drugs in particular, it is extremely important that there are no gaps in medication intake, otherwise the risk of acute events can often quickly increase without being noticed. If an emergency does occur, it is essential to react promptly. If, for example, you observe typical signals of heart failure, such as shortness of breath, chronic cough and swollen feet and legs, or typical signals of a heart attack, such as chest pain, please do not hesitate and contact a doctor as soon as possible.
Why don’t patients stick to treatments?
There are various reasons for this, and it often happens unconsciously. Patients simply forget to take their medication due to the stress of everyday life, they do not take the importance of their treatment seriously, or they fail to remember or understand medical information. Often, patients also lose track of which medication is due, when and how, because they have to take many different drugs.
Cardiac patients in particular often suffer from a variety of comorbidities and risk factors that are treated with many different drugs. Of course, this places great demands on the patients – and sometimes even overwhelms them.
Are there other factors influencing treatment adherence among patients?
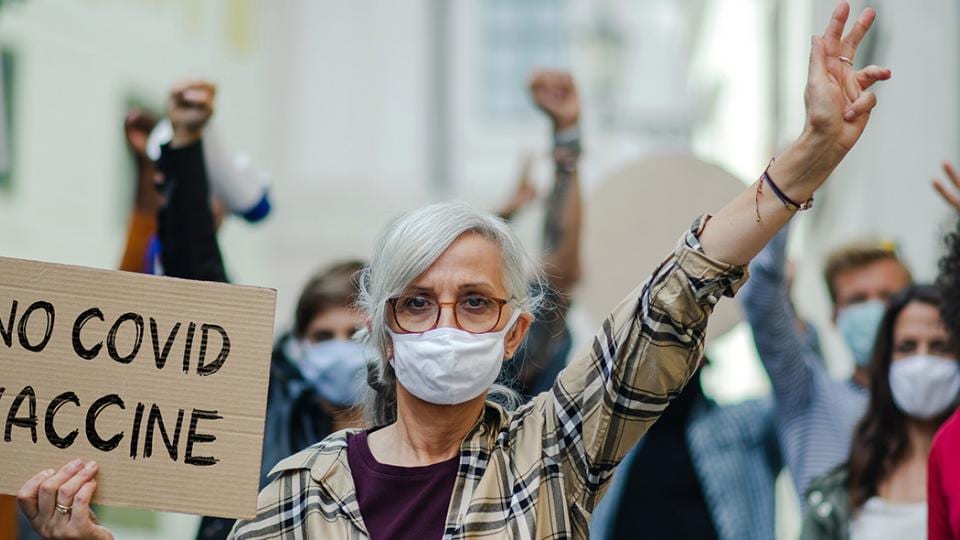
Media coverage and social media also have an impact on treatment compliance. If negative reports are made, it can happen that patients are doubtful of the safety of their medication. At the beginning of the pandemic, for example, there were reportedly reports that the use of certain drugs to treat high blood pressure were responsible for an increased risk of infection and more severe COVID-19 symptoms. Other studies then showed the opposite, however. This can lead to uncertainty among patients and may cause them to simply stop taking their medication without consulting a doctor. They are often not even aware of the consequences or the risk that they are taking, as they do not always see a physical reaction and immediate benefit when they take preventive therapies, as they do when they take a headache tablet, for example.
This is because cardiovascular drugs are often used for prevention. We treat risk factors to prevent the disease from manifesting in the first place, or to prevent an acute event such as an emergency hospitalization or stroke.
The awareness that patients put themselves in dangerous situations if they do not follow a prescribed therapy is, in my opinion, often underrepresented in the media. I therefore believe we need to raise greater awareness of the benefits for the patient and emphasize the importance of treatment adherence for ensuring treatment is successful.
What I would like to emphasize in this context is that all available drugs have been tested in large-scale studies and carefully scrutinized by regulatory authorities. And only drugs that have shown their effect in studies and are tolerable for the patient may be prescribed by doctors. Patients can rely on that. This is exactly what the regulatory authorities’ therapy guidelines are for – and if you are unsure, the first port of call should always be your treating doctor. In this respect, the importance of a trusting relationship between doctor and patient plays an even greater role.
What is your advice to patients – how can they improve their treatment adherence?
The simplest tips to ensure a correct intake of medicine include using boxes in which the medicines are sorted by day, sometimes also by time of day, or lists that are checked off and remind you to take your medication regularly.
It is best to schedule doctor’s appointments well in advance – then they have a permanent place in the calendar. Ideally, patients should prepare for their doctor’s visit, for example by noting down their questions and changes in their state of health so they can discuss them with their doctor. There are also checklists that can help the patient prepare.
Digital health support will also play an increasingly important role in supporting treatment adherence. Apps that remind people to take medication are already available today. In addition, a wide variety of approaches are also being investigated. For example, essential patient data such as blood pressure, blood values, heart rate, etc. are recorded via monitoring devices and can then be discussed with the doctor in video conferences. This enables close dialog between doctor and patient – even if they are no longer as mobile as they once were, say because of their illness or age.
You mentioned coronavirus earlier – what influence is the pandemic having on cardiovascular diseases?
Especially at the beginning of the COVID-19 pandemic, we observed that more and more patients were avoiding medical contact out of fear of becoming infected or not being able to be visited – be it for check-ups or emergency situations. As a result of late treatment, this unfortunately led to unfavorable courses and events that would have been avoidable, regardless of an infection. As I mentioned at the beginning, it is extremely important to call the emergency services if you suspect a heart attack or stroke – in such emergencies, it is vital to react quickly, because every minute counts.
One area that has less to do with treatment adherence, but is currently heavily researched, is the long-term aftereffects of COVID-19, which are grouped under long COVID. The effects on the heart are also being examined – an important topic that we are concerned with and that we need to understand even better.
Thank you for this interview, Mr. Roessig. Is there anything else you would like to tell readers?
At this point, I’d like to stress a very crucial piece of advice – keep your doctor’s appointments. This is especially true for patients with chronic diseases. Many things can be postponed, but visits to the doctor are not one of them.
Finally, I would like to emphasize one more thing. All available drugs have been extensively tested and their risk-benefit ratio has been proven by the authorities. If you cannot cope with your medication or have heard something negative about it, do not just stop taking it on your own initiative without asking your doctor. Instead, please speak to your doctor, with whom you can discuss this information and who can be sure to find an alternative or adjust the medication. This is probably the best way to improve treatment adherence.
Treatment adherence
Treatment adherence describes following the recommendations of the prescribing physician. This includes the dosage of a medication, taking tablets regularly, attending regular check-ups with the doctor, and responding appropriately in an emergency.
Medication adherence is the extent to which a patient adheres to the prescribed dose and interval of their treatment regimen. The first mention of the word “compliance” in medical literature appeared in 1966. In 2000, the word “adherence” became preferred over the word “compliance” among experts. Most studies on nonadherence come from endocrinology and cardiovascular medicine, but the overall nonadherence rate for both acute and chronic care combined, across all areas of medicine, is 40%.

Lothar Roessig received his MD from Hannover Medical School, Germany. He is board-certified in cardiology and internal medicine and works as a lecturer in medicine at Goethe University Frankfurt, Germany. As an interventional cardiologist and member of the faculty at the University Hospital Frankfurt, he was an investigator in numerous clinical trials until 2007, when he transitioned to the clinical research industry. In 2009, Roessig joined Bayer, where he is currently Vice President, Head of Clinical Development in the Therapeutic Area Cardio-Renal.